8 great NHS initiatives you’ve probably never heard about
People are coming up with innovative solutions to patient problems all the time. In collaboration with Imperial College Health Partners, we celebrate eight national initiatives putting people at the heart of the service
1. Care navigators
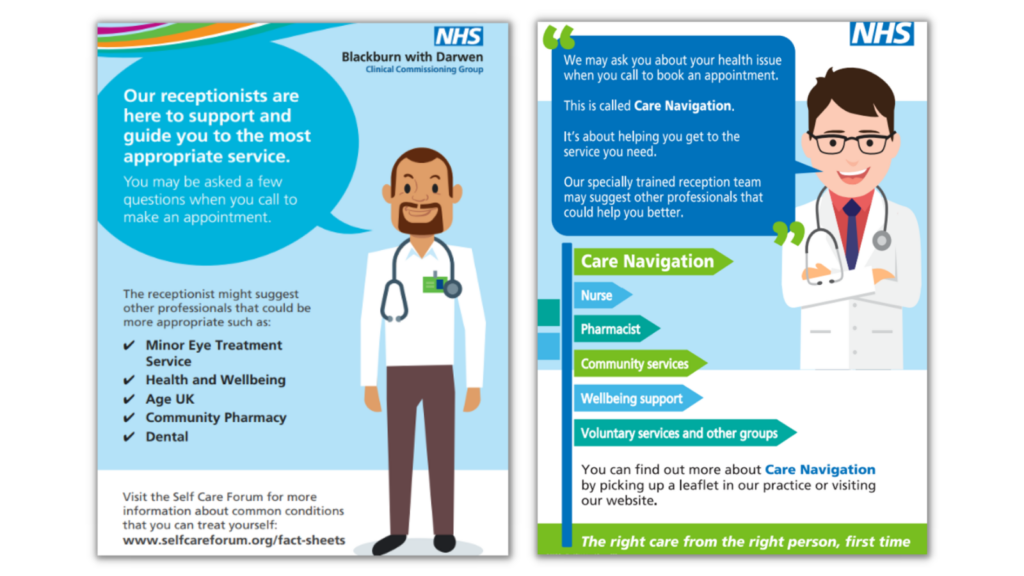
How does it work?
Care Navigators are trained staff who can help direct patients to the most appropriate service or person depending on their needs.
The role is often carried out by non-clinical front-line staff such as receptionists, patient liaison officers or volunteers.
The aim is to remove the onus from the patient and to support them to access the most appropriate service first-time.
2. No Wrong Door

How does it work?
No Wrong Door is an approach to delivering mental health services that aims to ensure that individuals are supported. So they can access the help they need when they need it, regardless of where they first turn for help.
The model involves GPs, local authorities, community services and the voluntary sector working together to meet the physical, mental and social needs of service users in a coordinated way.
3. The NHS e-Referral Service
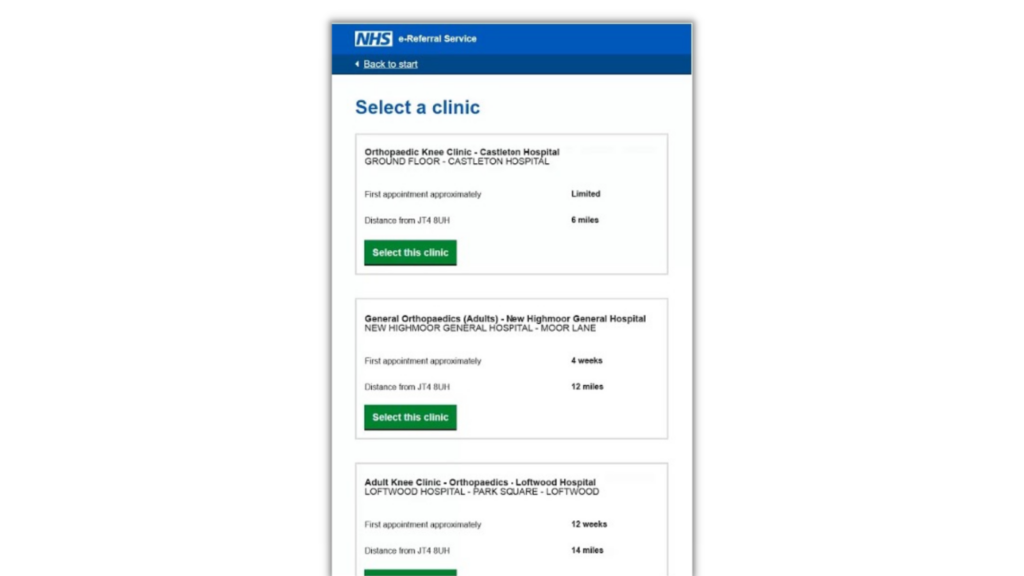
How does it work?
The NHS e-Referral Service (e-RS) supports referrals to secondary care (hospitals or specialist clinics) from GPs.
The patient-facing part of the service – Manage Your Referral – is available on the NHS website and via the NHS App. There is also a low-cost telephone service for patients who would prefer not to book online.
The service allows patients to track the status of referrals and schedule appointments. When making these bookings, patients are given the option to select a time, date or place of their choice.
4: Patients Know Best
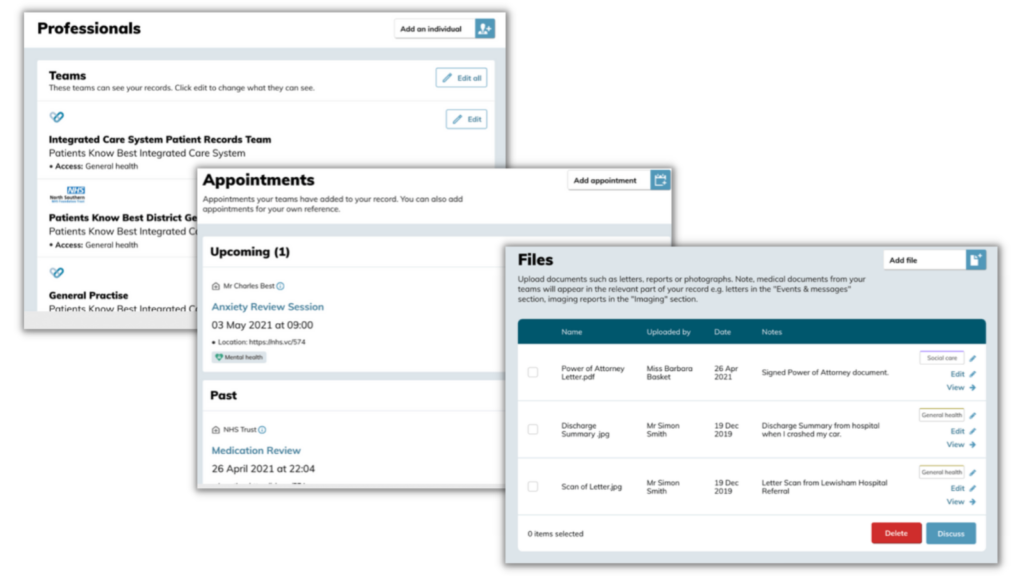
Patients Know Best is an online service that gives patients secure access to their health record. It links to the NHS App and is designed to improve how patients experience and access NHS services and information.
The platform enables patients to see their appointments, test results, medication lists and care plans together in one place.
Patients can choose to share information with carers and clinicians so that everyone looking after them understands the type of care and support they need and want.
5. Connecting Care for Children

Connecting Care for Children is a workforce model which brings together paediatric specialists – such as consultants, school nurses, early years teams and health visitors – together with GPs to care for children in their area.
The model involves regular joint meetings between these professionals, where complex cases can be discussed in a collaborative way. GPs also have a telephone hotline they can call for paediatric advice in between.
This partnership approach aims to support GPs to continue caring holistically for children in community settings, reducing the need for onward referrals.
6. RIXWiki

How does it work?
RIX Wiki is an online portal that enables young adults with learning disabilities to share their needs, goals, and preferences.
Wikis are simple, secure and easy to build personal webpages where users can upload photos, videos and documents to help tell their story. This can help to improve understanding of what matters most to the person and what works best.
The aim is to support person-centred care where professionals get to know individuals on their own terms rather than through a service lens.
7. Patient Check.In
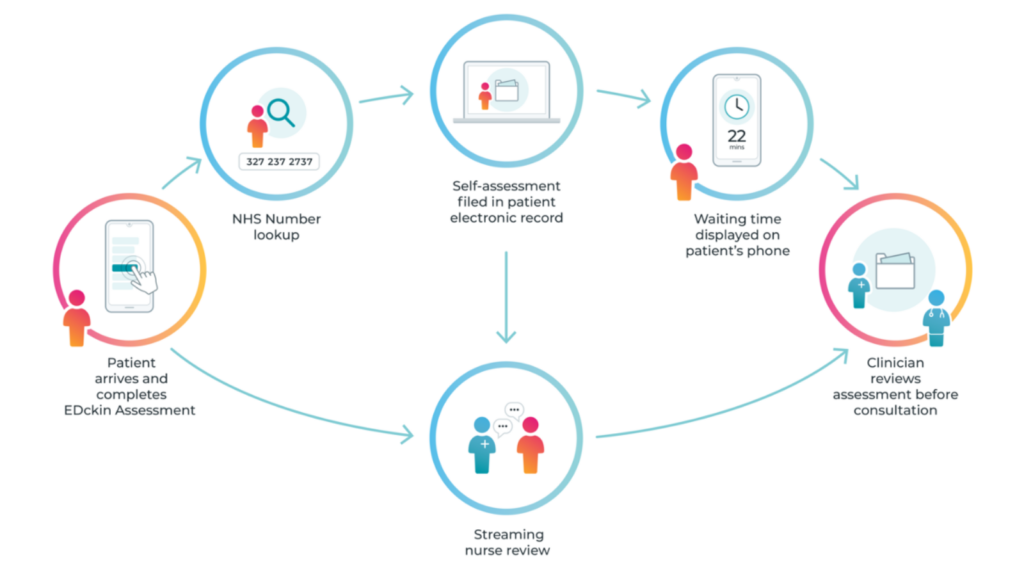
How does it work?
Patient check.in is a check-in process which allows patients in A&E to see real-time updates of their position in the queue and their likely wait time.
On arrival, patients complete a brief questionnaire, which enables them to tell clinicians why they are in the emergency department in their own words.
Once registered, patients can monitor their position in the queue either on their phone or on TV screens in the waiting room.
Having this waiting time information readily available aims to help manage patient expectations. It also reduces anxiety around being forgotten, passed over or missed.
8. Hospital discharge checklist
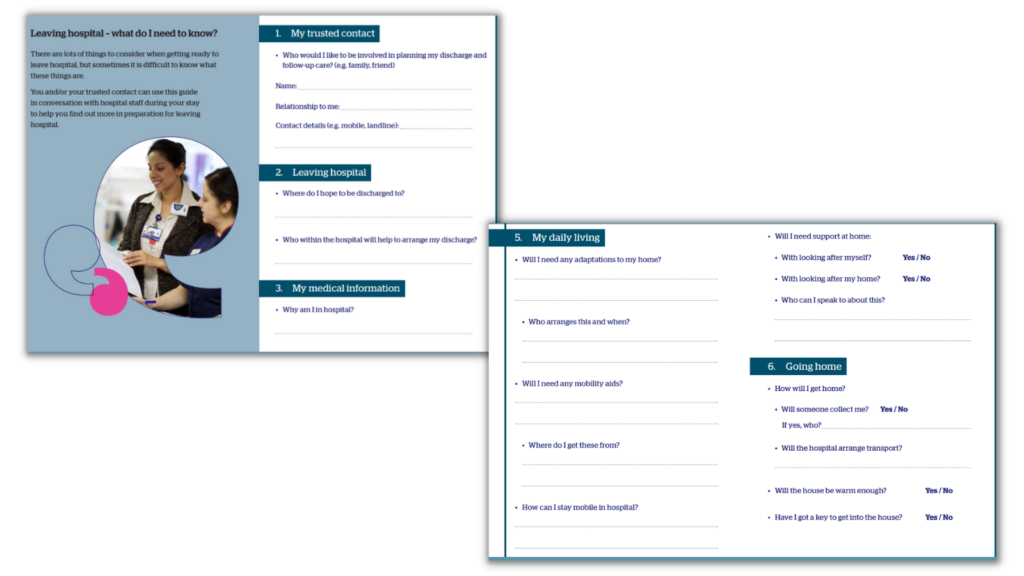
How does it work?
There are lots of things to consider when getting ready to leave hospital. But sometimes it is difficult to know what these things are – particularly for older people, who often have multiple conditions and are under the care of several providers.
This checklist aims to guide patients and carers in their conversations with hospital staff. It ensures they know the important information to ask for and are able to record it before being discharged.
It also reflects the most common questions posed by patients when leaving hospital. Including symptoms to look out for, changes to medication, and plans for getting home.

Engage Britain has been asking people for their experiences and views of the NHS and care. Find out how they settled on the key problems before developing detailed solutions… read more

How can we help solve the biggest challenge facing the country? Here’s a whistle-stop tour of our approach to make change happen… read more

We’re a fully independent charity that gives people a say on what matters most to them. We can make our…read more