Welcome to the second of our three part series taking you inside The People’s Panel on health and care.
It was important for the Panel to hear about people’s health and care experiences across the country. So they watched stories shared by people during Community Conversations. They also had the opportunity to ask any burning questions of health and care experts, to help fill gaps in their knowledge.
What Part 2 covers:
- Listening to conversations about health and care
- Answering the Panel’s burning questions
- About funding: ‘How is money spent in the NHS?’
- About inequality: ‘Communities can do more for themselves’
- About the workforce: ‘Why are there staffing shortages?’
- The Panel’s reflections
Listening to conversations about health and care
In the months leading up to The People’s Panel, around 700 people took part in Community Conversations online to discuss their health and care experiences – what they felt was working and what could be better. A selection of video recordings were shared with the Panel to reflect upon.
The Panel’s reflections
Hazel, Panel member
Harry, Panel member
Ray, Panel member
Answering the Panel’s burning questions
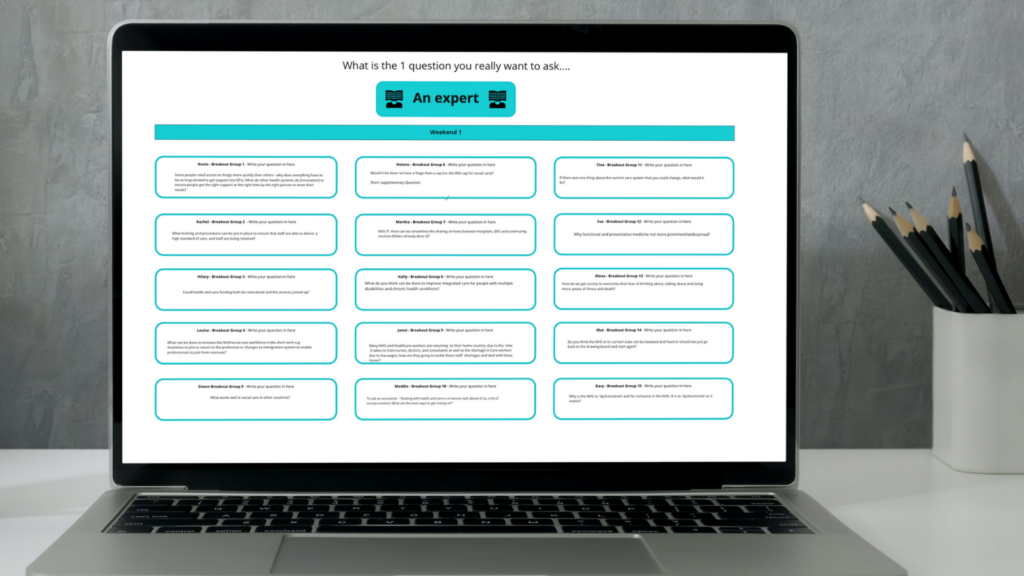
As the Panel reflected on what they’d heard, naturally lots of questions came up. They decided together what they needed more information about. Engage Britain then brought in experts to answer their burning questions, which included:
- What’s the money being spent on and how could it be spent better?
- How can we improve access to health and care for everyone?
- How can we tackle staff shortages, poor working conditions and care worker pay?
Below is a selection of what the experts shared (and some of the Panel reactions). Or you can watch the guest speaker presentations in full here.
Funding: ‘How is money spent in the NHS?’
(Richard Douglas, Chair of the South East London Integrated Care System)
RICHARD DOUGLAS (South East London ICS): Here’s a whistle stop tour of the NHS numbers.
- Where is the money spent? In 2021 about £150 billion was spent on the NHS in England. That’s £3,000 for each and every person in the country. It’s almost half of our public service spend. And it’s grown massively in the last 20 years: in 2000, we spent £60 billion.
- Who decides where and how the money is used? There’s a distribution across the country to each locality. It’s done on a formula basis, driven by how many people live in each area and what the health needs are. The aim is to give a fair share of health resources per head everywhere in the country.
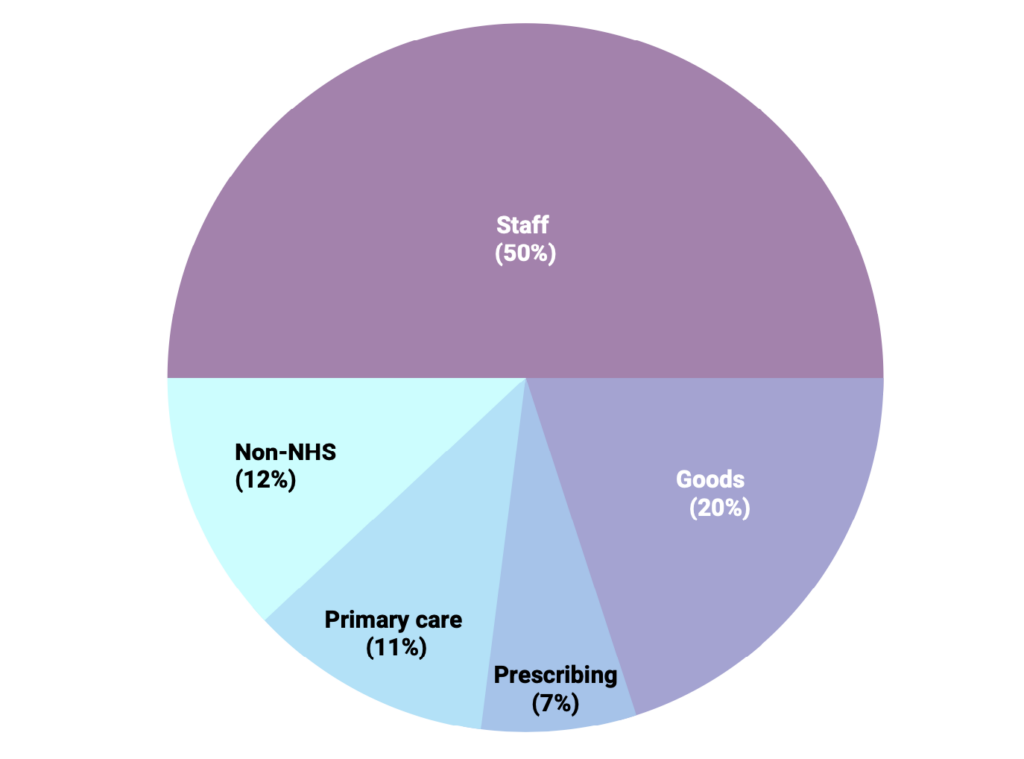
- How is the money spent? Most contacts are with primary care – GPs, pharmacists, opticians and dentists. But only about £1 in £5 is spent in that area. The rest is primarily spent on hospitals. They account for somewhere between 65% and 75% of spending in the NHS.
Over half the NHS budget goes on staff. It’s largely a people business.
RICHARD DOUGLAS, SE LONDON INTEGRATED CARE SYSTEM
Funding: ‘We’ve lost sight of the individual at the heart of care’
(Professor Chris Jones, Deputy Chief Medical Officer, Welsh government)
CHRIS JONES (Welsh government): Since I qualified as a doctor 40 years ago, life expectancy has increased by 10 years. And the typical 80 year old has multiple conditions. But we still treat each condition separately. We’ve lost sight of the individual at the heart of care. We should not assume that survival is more important than quality of life.
Inequality: ‘Communities do more when they decide for themselves’
(Samira Ben Omar, Head of Engagement, North West London Clinical Commissioning Group)
SAMIRA BEN OMAR (North West London CCG): Communities and faith spaces are the lifeblood of local action. Every conversation I’ve ever had about health always veers towards good secure employment, good secure housing. Health happens in communities not in the healthcare system.
Inequality: ‘We’ve got to match the right thing to the patient need at the time’
(Robert Varnam, Head of GP Practice Development, NHS England and a GP)
ROBERT VARNAM (GP, NHS England): There is no one-size-fits-all way of doing healthcare. And it’s not good for people. There should not be an insistence that everyone has the same kind of appointment, with the same kind of healthcare practitioner. Hospital doctors have risen three time faster than the number of GPs, at a time when what society actually needs is more GPs.
Inequality: ‘Demand for mental health support is growing’
(Tom Pollard, Mental Health Social Worker)
TOM POLLARD (Mental Health Social Worker): Mental health needs to be understood as deeply social, as opposed to being primarily medical. There’s still far too much focus on medication and managing systems. And not enough on supporting people to address the issues in their lives.
Workforce: ‘Why are there staffing shortages?‘
(Rachel Hollis, Chair of Royal College of Nursing’s Professional Nursing Committee)
RACHEL HOLLIS (Royal College of Nursing): Shortages are a chronic issue. Nurses returning to their home country have had an impact. Also nurses coming to the UK from the EU have dropped 90% since 2016. Domestically, we have not trained enough nurses. We’re often led by what can be afforded rather than looking at demand, which will continue to grow.
Workforce: ‘Why are so many staff leaving adult social care?’
(Leire Agirre, Principal Social Worker, Central Bedfordshire Council)

LEIRE AGIRRE (Principal Social Worker): Turnover in the care sector is particularly high, with nearly a third of the workforce changing job each year. That’s usually to do with better working conditions.
Let’s look at the average pay for a care worker versus that of somebody working in a supermarket:
- The average pay for a care worker is £9 an hour. That is only 10p more than the minimum wage
- The King’s Fund found that seven out of the largest supermarkets actually pay more than what’s paid in social care, roughly about two pounds more per hour
- if you then look at reasons for staying in the sector, a carer working for 20 years with a lot of experience only gets paid about 15p more an hour
So there’s very little incentive, even if it’s a ‘love’ job. And carers have a lot of dedication. But to stay in a career long-term, people want a fair level of pay.
Those working in the social care system are not valued. As a society we do not value the carer.
LEANNE, PEOPLE’S PANEL MEMBER
The Panel’s reflections
BECKY (Panel member): “Hearing from a number of experts in NHS and social care really helped us understand what the issues were.”

